Hope Ngumezi wrapped a blanket around his wife as she grieved the loss of her 11-week pregnancy. He couldn’t help but wonder why no obstetrician had come to see her.
Porsha Ngumezi spent a grueling six hours in the emergency department at Houston Methodist Sugar Land on June 11, 2023. During her time there, she lost so much blood that she required two transfusions. Despite her eagerness to return home to her young sons, the nurse’s notes indicated that she was still experiencing the passage of large clots, comparable in size to grapefruits.
Hope called her mother, who used to be a doctor, and her mother was very clear in her advice. She said, “You need a D&C,” referring to a procedure called dilation and curettage. This procedure is commonly performed for first-trimester miscarriages and abortions. By removing the remaining tissue from her uterus, the doctor could stop the bleeding.
When Dr. Andrew Ryan Davis, the attending obstetrician, finally arrived, he informed Hope that it was standard procedure at the hospital to administer a medication called misoprostol to facilitate the passing of tissue. Hope had faith in the doctor’s expertise and Porsha followed the instructions by taking the pills. However, despite this, the bleeding persisted, as documented in the records.
Her heart came to a halt three hours later.
According to a detailed summary of her case reviewed by more than a dozen doctors for ProPublica, the death of the 35-year-old could have been avoided. These medical professionals argue that the incident raises significant concerns about the impact of abortion bans on doctors, pushing them to deviate from standard care and resort to less-effective alternatives that could potentially put their patients at higher risk. In fact, doctors and patients in the state have reported witnessing similar decisions being made.
According to medical experts, it was evident that Porsha urgently required an emergency D&C. She was experiencing severe bleeding, and the doctors were aware of her blood-clotting disorder, which significantly increased the risk of excessive and prolonged bleeding. Dr. Amber Truehart, an OB-GYN at the University of New Mexico Center for Reproductive Health, explained that administering Misoprostol at 11 weeks would not be effective in stopping the bleeding quickly enough. This would leave the patient at a higher risk of developing hemorrhagic shock. The cause of death, as determined by the medical examiner, was hemorrhage.
D&Cs are considered a crucial aspect of maternal healthcare as they have the potential to save lives. During the procedure, doctors gently insert a straw-like tube into the uterus and suction out any remaining pregnancy tissue. This process allows the uterus to empty and subsequently close, effectively stopping any bleeding.
Dilation and curettage (D&C) is a medical procedure that is not only utilized for therapeutic purposes, but also to terminate pregnancies. However, due to the association with abortion, state laws have been enacted to regulate and restrict its use. In Texas, for instance, doctors who defy these stringent regulations may face a prison sentence of up to 99 years. Sadly, ProPublica has documented five cases in which women lost their lives as a result of not receiving a D&C or its alternative procedure, dilation and evacuation (D&E), during the second trimester of pregnancy. Disturbingly, three of these fatalities occurred in Texas.
According to Texas doctors interviewed by ProPublica, the perception of the procedure has changed due to the law, with some no longer considering it as the first-line treatment. This shift in perspective is attributed to concerns about potential legal repercussions and the additional documentation and hospital approval required for performing a D&C after a miscarriage. ProPublica’s investigation revealed that this change in approach has occurred even in cases like Porsha’s, where there is no fetal heartbeat or when the circumstances should qualify for an exception under the law. As a result, some doctors are transferring these patients to other hospitals, causing delays in their care, while others are resorting to alternative treatments that may not align with the medical standard.
Misoprostol, the medication administered to Porsha, is a reliable method for completing low-risk miscarriages. However, it is not advisable to use this drug when the patient’s condition is unstable. Although Misoprostol is commonly used as part of a two-pill regimen for abortions, its administration may attract less attention compared to a D&C procedure. This is due to the fact that it requires a smaller medical team and is frequently used to induce labor and treat postpartum hemorrhage. In recent years, there have been instances in Texas where women experiencing heavy bleeding during a miscarriage have come forward, stating that they were only given medication when they specifically requested a D&C. In one distressing case, a woman even fainted in a pool of her own blood.
According to Dr. Alison Goulding, an OB-GYN in Houston, there is a significant stigma and fear associated with D&Cs that does not exist with misoprostol. In Texas, doctors tend to avoid recommending D&Cs, even in cases where it would be the standard procedure, due to the perception that it is associated with abortion, which is illegal. This fear and stigma prevent many individuals from accessing the necessary healthcare they require.
The doctors and nurses responsible for Porsha’s care did not respond to multiple requests for comment.
When reviewing the summary of Porsha’s case, multiple physicians noticed that the post-mortem notes by Davis failed to acknowledge the documented concerns of the nurses regarding Porsha’s “heavy bleeding.” Surprisingly, after Porsha’s demise, Davis claimed that the nurses and other providers described the bleeding as “minimal,” despite no such statements being recorded by the nurses. ProPublica attempted to reach out to Davis to address this inconsistency, but he did not respond to any form of communication including emails, texts, and calls.
Houston Methodist officials were unresponsive to a comprehensive list of inquiries about Porsha’s treatment. When asked if Davis’ approach was standard procedure at the hospital, they refrained from offering any comments. However, a spokesperson did mention that the care provided to each patient is tailored to their specific needs.
According to the spokesperson, Houston Methodist hospitals abide by all state laws, including the existing abortion law in Texas.
“We Need to See the Doctor”
This Article Includes
Hope was amazed by the boundless energy that Porsha had when it came to their two young sons, aged 5 and 3. Whenever Porsha wasn’t occupied with work, she could be found enthusiastically chasing the boys around the house or joyfully dancing with them in the living room. Being the finance manager for a charter school system, Porsha took charge of managing the household budget. Meanwhile, as an engineer at an airline, Hope had the opportunity to take their children on exciting flights to various destinations across the globe, including Chile, Bali, Guam, Singapore, and Argentina.
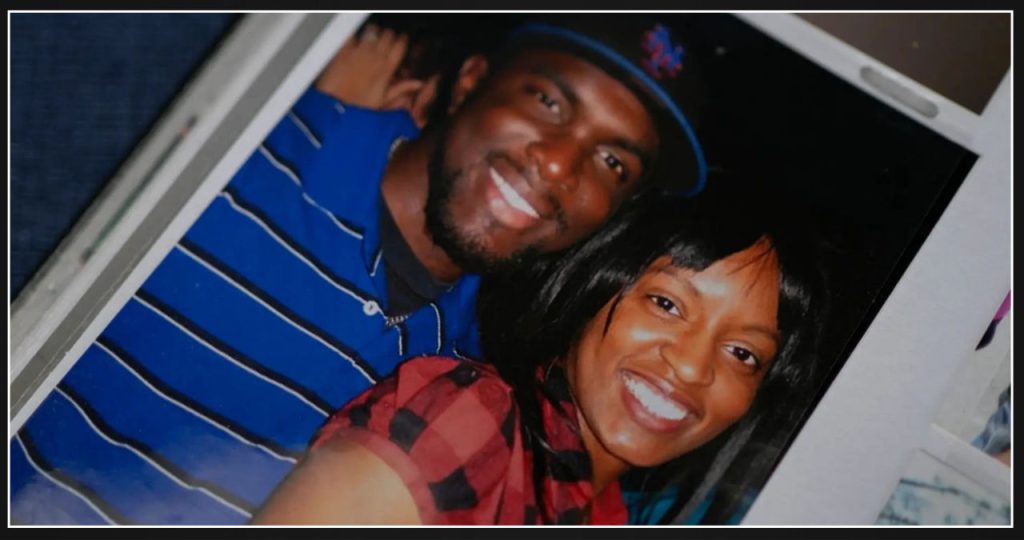
Hope and Porsha first crossed paths at Lamar University in Beaumont, Texas. Reflecting on their early days, Hope shared, “When Porsha and I started dating, I knew right away that I was going to fall in love with her.” Porsha’s magnetic personality and ambition were evident, as she went on to earn an MBA. However, what stood out to Hope was her gentle and caring nature, always looking out for his emotional well-being. Coming from large families themselves, the couple shared a common desire to create a family of their own.
When Hope found out that Porsha was pregnant again in the spring of 2023, he had a strong desire for a girl. To ensure a smooth pregnancy journey, Porsha sought the expertise of a new OB-GYN who could accommodate her after 11 weeks. However, at the tenth week, Porsha started to experience spotting. Concerned, she reached out to her obstetrician who advised her to go to the emergency room if the situation worsened.
Porsha and Hope decided to celebrate the end of the school year by taking their boys to a water park in Austin. As they were heading back on June 11, Porsha informed Hope that the bleeding had gotten heavier. Understanding the urgency, they made a plan. Hope would stay home with the boys until a relative could take over, while Porsha drove to the emergency room at Houston Methodist Sugar Land. This hospital is one of the seven community hospitals that are part of the Houston Methodist system.
By 6:30 p.m, three hours after Porsha had arrived at the hospital, she noticed large clots in the toilet. The emergency physician described it as “significant bleeding.” Concerned, Porsha immediately texted Hope, informing her about the situation. Around 7:30 p.m, Porsha messaged Hope again, sharing that the nurse mentioned the possibility of surgery if the bleeding didn’t stop. At 7:50 p.m, after having her second diaper changed within an hour, Porsha urgently requested Hope to come to the hospital.
According to records, the doctor did not mention a D&C at this stage. Medical experts have noted that this cautious approach has become more prevalent due to abortion bans. In the absence of clear indications of significant risk, hospital administrators have instructed physicians to closely monitor patients. Dr. Robert Carpenter, a maternal-fetal medicine specialist working in multiple hospital systems in Houston, revealed that Methodist has not disclosed its miscarriage protocols or provided guidance to doctors regarding the abortion ban.
Porsha patiently waited for Hope, while a radiologist conducted an ultrasound examination. The radiologist observed that Porsha had a “pregnancy of unknown location,” with the scan revealing a sac-like structure but no fetus or cardiac activity. Based on these findings and Porsha’s symptoms, it was evident that she was experiencing a miscarriage.
According to several doctors who spoke with ProPublica, the ultrasound record alone was not sufficient from a legal standpoint. Due to Porsha’s lack of prenatal visits, there was no documentation to confirm that she was 11 weeks pregnant. The diagnosis of a “pregnancy of unknown location” on paper could also indicate that she was in the early stages of a normally developing pregnancy, where cardiac activity would not yet be detectable. In Texas, abortion is prohibited from the moment of fertilization, so a record indicating the absence of cardiac activity is not enough for physicians to legally intervene.
Dr. Gabrielle Taper, an OB-GYN resident in Austin, has recently shared her experiences regarding delays in managing pregnancies of unknown location after ultrasound reports. She raises an important question about whether certain interventions would be considered abortions or not. The new abortion ban has resulted in increased uncertainty among medical professionals about when to intervene, how to determine if it is a miscarriage, and the appropriate waiting period before taking action. Medical practitioners are now more cautious and require stronger evidence to make definitive decisions.
Records show that at Methodist, the emergency room doctor contacted Davis, the on-call OB-GYN, to discuss the ultrasound findings. Together, they decided on a course of action which involved closely monitoring the bleeding through observation in the hospital.
Around 8:30 p.m., shortly after Hope arrived, Porsha lost consciousness. Filled with fear, he gently cradled her head in his hands, desperately attempting to revive her. “Babe, please look at me,” he pleaded. “Stay focused.” Her blood pressure had dropped to a dangerous level. Porsha had postponed accepting a blood transfusion until his arrival. Now, as she regained consciousness, she consented to receive one, followed by another.
Dr. Lauren Thaxton, an OB-GYN who recently left Texas, advises that completing the miscarriage is necessary in order to stop the bleeding.
Dr. Daniel Grossman, a professor of obstetrics and gynecology at the University of California, San Francisco, who reviewed Porsha’s case, expressed his shock at the situation. He emphasized that Porsha was experiencing significant blood loss, yet the physician did not take immediate action by performing an aspiration procedure.
At 9:45 p.m., nurse Esmeralda Acosta noted that Porsha was still experiencing the passage of large clots comparable to the size of grapefruit. Just fifteen minutes later, upon learning that Dr. Davis intended to transfer Porsha to a less staffed floor, Nurse Acosta expressed her concern about moving her out of the emergency room considering her condition, as documented in the medical records.
At 10:20 p.m., Davis finally visited Porsha after a long wait of seven hours. Hope recalled the advice his mother had given him over the phone earlier that night: “She needs a D&C.” However, the doctor appeared to have a different plan in mind. He expressed confidence in using misoprostol as the initial approach. If that didn’t prove successful, Hope vividly remembers the doctor saying that they would proceed with the procedure.
Porsha found the idea of surgery terrifying, so she was relieved when she heard about the option of taking a pill. Hope, on the other hand, wasn’t aware that a D&C didn’t involve any incisions, only suction, and that it would stop the bleeding faster. Davis failed to provide this information to them. Despite the lack of explanation, the Ngumezis trusted Davis’s recommendation without hesitation. Hope explained, “I assumed that since he was the OB, he had probably encountered this situation numerous times and knew what was best.”
Several doctors who examined Porsha’s case expressed their concerns about this recommendation. They believed that administering misoprostol to a woman experiencing heavy bleeding, especially one with a blood clotting disorder, could be dangerous. Dr. Elliott Main, a renowned expert in hemorrhage and the former medical director for the California Maternal Quality Care Collaborative, stated, “That’s not the appropriate course of action. She should have been taken to the operating room.” Main and other doctors emphasized the importance of providing patients with comprehensive information about the risks and benefits of all available options, including a D&C.
Performing a D&C, however, garners more attention from colleagues, creating a higher hurdle in states where abortion is illegal, according to Goulding, an OB-GYN in Houston. Staff members are familiar with misoprostol because it is commonly used for labor induction and only requires a doctor and nurse to administer. In contrast, performing a procedure like a D&C would necessitate finding an operating room, an anesthesiologist, and a nursing team. “You have to convince everyone that it is legal and won’t put them at risk,” Goulding explained. “Many people may be fearful and misinformed, leading them to refuse participation, even when it’s for a miscarriage.”
Davis transferred Porsha to a unit with a lower level of intensity, as stated in the records. Hope was curious as to why they were leaving the emergency room, considering the nurse’s apparent concern. Despite her reservations, Davis chose to comfort Porsha by gently rubbing her arms. Methodist Hospital had a good reputation, which made Hope feel more at ease with trusting the doctors.
Porsha started complaining of chest pain while they were on their way to the other ward. She kept mentioning it even after they arrived in the new room. Surprisingly, there are no nurse’s notes documenting the extent of her bleeding from this point onward. Concerned for his wife’s well-being, Hope informed a nurse that she didn’t feel right, recalling that the last time she said that, she passed out. Though furious, he did his best to remain composed in order to not alarm Porsha, insisting that they needed to see the doctor.
According to several physicians, ProPublica found that even though a pregnant patient’s vital signs may appear normal, their bodies have the ability to compensate for a significant period of time before experiencing a sudden decline. Therefore, any indication of distress, such as chest pain, should not be overlooked and should prompt further investigation through tests like an electrocardiogram or X-ray. Porsha’s case serves as a reminder to healthcare professionals of the critical importance of intervening before a life-threatening emergency arises.
According to records, no tests were ordered by Davis.
At around 1:30 a.m., Hope sat by Porsha’s bed, placing his hands on her chest, assuring her, “We will find a solution for this.” They discussed breakfast options when suddenly, Porsha started gasping for air.
Frantically, he cried out for assistance over the intercom, desperately pleading, “I need help! She’s struggling to breathe.”
“All She Needed”
After a long day, Hope arrived home feeling lost and bewildered. One of his sons asked if their mother was still at the hospital, and Hope simply nodded, unable to find the right words to convey the heartbreaking truth. He went about his usual routine of getting the boys dressed and driving them to school, as if the previous day had been nothing more than a terrible nightmare. When he reached for his phone to call Porsha, as he did every morning after dropping off the kids, reality hit him once again – he couldn’t make that call anymore.
Friends continued to reach out to offer their condolences. Many of his family’s connections were in the medical field, and they all echoed similar sentiments. One person suggested that all she needed was a D&C, while another said that she shouldn’t have been given that medication. The callers reassured him that it was a simple procedure, emphasizing that it is routinely performed in Nigeria.
Since the death of Porsha, multiple families in Texas have come forward to share their similar experiences. In one instance this May, Ryan Hamilton’s wife experienced bleeding while miscarrying at 13 weeks. The first doctor they consulted at Surepoint Emergency Center Stephenville observed no fetal cardiac activity and prescribed misoprostol, as documented in the medical records. However, when they returned due to worsening bleeding, an emergency doctor named Kyle Demler stated that he couldn’t take any action due to “the current stance” in Texas. Hamilton recorded his recollection of the conversation shortly after speaking with Demler. Despite multiple requests for comment, Surepoint Emergency Center Stephenville and Demler did not respond.
Physicians throughout Texas are attributing interference with medical care to the law. Following ProPublica’s report on two women who died due to delays in miscarriage care, 111 OB-GYNs sent a letter to Texas policymakers, expressing their concerns that “the law does not permit Texas women to receive the essential and life-saving care they require.”
Even women who fall under the exceptions mentioned in the law are experiencing delays and refusals due to the severe criminal penalties. To illustrate, legislators made an amendment last year to allow patients diagnosed with previable premature rupture of membranes (when a patient’s water breaks before the fetus can survive) to be exempt from the ban. However, doctors can still face prosecution for providing abortions in these cases, although they are given the opportunity to defend themselves with what is known as an “affirmative defense,” similar to a murder suspect claiming self-defense. Despite this small change, some doctors choose to transfer these patients to other hospitals instead of treating them. Dr. Allison Gilbert, an OB-GYN in Dallas, shared that doctors refer these cases to her because they don’t feel comfortable proceeding with the abortion themselves. This situation is frustrating as it prevents timely action for clearly emergent cases. Furthermore, women who are denied treatment for ectopic pregnancies, another exception in the law, have filed federal complaints.
Houston Methodist has an ethics committee in place to assist physicians and patients in making appropriate decisions regarding miscarriage management. According to Gale Smith, a spokesperson for the hospital, the committee is usually able to provide guidance within hours, ensuring compliance with state laws.
In the medical record, Davis described the patient’s condition after Porsha’s death. According to him, the patient appeared stable, with mild bleeding and no signs of distress. Davis ordered bloodwork to ensure that the patient was not experiencing concerning bleeding. However, medical experts who reviewed Porsha’s case found discrepancies in Davis’ documentation. They noted that the nurse and other providers reported decreasing bleeding, contrary to what Davis had documented. Additionally, Davis did not mention the heavy bleeding that the nurse had clearly documented, including the significant bleeding that led to the blood transfusion. This lack of documentation surprised Grossman, a UCSF professor.
Patients experiencing a miscarriage are often left uncertain about what to anticipate during their time at Houston Methodist.
In May of this year, Marlena Stell, a patient experiencing symptoms similar to Porsha, sought treatment at Houston Methodist The Woodlands Hospital. Like Porsha, Marlena was 11 weeks pregnant and experiencing heavy bleeding. Medical records showed that an ultrasound revealed no fetal heartbeat and indicated an incomplete miscarriage. Marlena expected that the medical staff would take necessary measures to stop the bleeding.
Instead, she spent hours bleeding at the hospital. She requested a D&C procedure to remove the remaining tissue, but the doctor administered methergine instead. Methergine is typically used to stop bleeding after childbirth, but it is not the standard treatment for a miscarriage, according to doctors interviewed by ProPublica. Dr. Jodi Abbott, an associate professor of obstetrics and gynecology at Boston University School of Medicine, reviewed the records and stated, “She experienced heavy bleeding, and her ultrasound indicated retained products of conception. The standard procedure in this case would be a D&C.”
According to Stell, she was instructed to go home and allow the miscarriage to happen naturally instead. Later that night, she experienced a complete miscarriage. However, doctors who assessed her case, which was similar to Porsha’s, emphasized the risk that physicians take when they deviate from the standard of care. Abbott stated, “She was fortunate – she could have lost her life.” Houston Methodist did not provide a response regarding Stell’s treatment.
Hope never considered that the laws regarding abortion could impact his wife’s miscarriage until now. It seems to be the only explanation that makes sense to him. According to Hope, instead of enacting legislation to ensure safer pregnancies, we have implemented laws that actually pose a risk to them.
For months, Hope’s youngest son struggled to comprehend the absence of his mother. Porsha’s hair had been neatly braided, and whenever the toddler spotted a woman with similar braids from a distance, he would excitedly chase after her, exclaiming, “That’s mommy!”
A few weeks ago, Hope embarked on a journey to Amsterdam in search of peace of mind. It was his first solo trip, and as he strolled through the city, he couldn’t help but feel lost without Porsha by his side. Every step reminded him of how much she would have enjoyed the festive Christmas lights and eagerly sampled the delectable pastries. He imagined her playful teasing when he dozed off during a boat tour of the picturesque canals. Hope poured his thoughts into his journal, expressing his hope that this getaway would provide solace. However, instead of finding solace, he found himself constantly envisioning Porsha’s presence next to him.